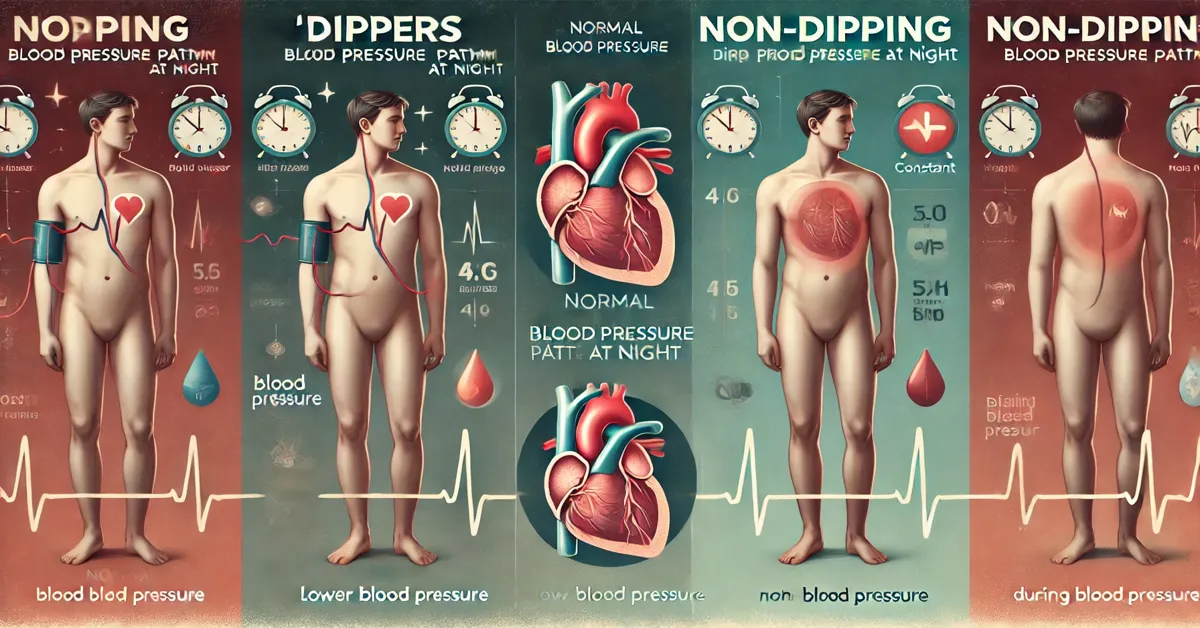
dipper and non dipper blood pressure, a critical measure of cardiovascular health, follows a rhythmic pattern over a 24-hour period. For most individuals, blood pressure is not constant throughout the day and night, but instead varies in response to the body’s circadian rhythm. This fluctuation gives rise to two distinct groups based on nocturnal blood pressure patterns: “dippers” and “non-dippers.” The classification into these categories has significant implications for understanding cardiovascular risk, managing hypertension, and guiding treatment strategies.
In this article, we will explore the concept of dippers and non-dippers, the physiological mechanisms behind blood pressure variations, the associated risks and conditions, and management strategies for individuals in both categories. We will also delve into the importance of blood pressure monitoring and offer insight into lifestyle and medical interventions that can support heart health.
Understanding Circadian Rhythm in Blood Pressure
The circadian rhythm is a natural, internal process that regulates the sleep-wake cycle and repeats roughly every 24 hours. It influences many bodily functions, including hormone release, metabolism, and blood pressure. During the day, physical activity, stress, and environmental factors cause blood pressure to rise and fluctuate. At night, while sleeping, blood pressure typically drops due to decreased activity and a slower heart rate.
This normal dip in blood pressure during sleep is referred to as “nocturnal dipping.” In a healthy individual, blood pressure typically falls by about 10-20% compared to daytime values. This reduction in blood pressure during sleep allows the heart to rest and recover from the day’s exertions, contributing to overall cardiovascular health.
However, in some individuals, this natural dip does not occur, or the drop in blood pressure is less pronounced. These individuals are classified as “non-dippers.” The absence of a significant drop in blood pressure during the night can increase the risk of cardiovascular events, such as heart attack or stroke, and is associated with greater overall cardiovascular strain.
Dippers: Normal Nocturnal Blood Pressure Patterns
Individuals who experience the expected decrease in blood pressure at night are classified as “dippers.” This group sees a 10-20% drop in their blood pressure during sleep, which is considered the norm. Dippers are generally believed to have a lower risk of cardiovascular events compared to non-dippers because their blood pressure pattern allows the heart to recover during rest periods.
Characteristics of Dippers:
- Nocturnal Blood Pressure Reduction: Dippers experience a significant drop in blood pressure during sleep, typically within the range of 10-20%.
- Lower Cardiovascular Risk: The regular dip in blood pressure is protective, reducing the strain on the cardiovascular system during nighttime.
- Healthy Circadian Rhythms: The presence of a dipping pattern suggests that the individual has a well-regulated circadian rhythm, with normal hormonal and metabolic cycles that support heart health.
For dippers, maintaining this healthy pattern is essential for long-term cardiovascular well-being. Regular monitoring of blood pressure can help ensure that the dipping pattern remains consistent, particularly as people age or if they are diagnosed with conditions that could affect their cardiovascular system.
Non-Dippers: Abnormal Nocturnal Blood Pressure Patterns
Non-dippers are individuals whose blood pressure does not decrease by the expected 10-20% during sleep. Some non-dippers may experience a slight reduction in blood pressure at night, while others might see no reduction or even an increase in nighttime blood pressure levels.
Characteristics of Non-Dippers:
- Lack of Nocturnal Blood Pressure Reduction: Non-dippers either experience a very slight decrease or no decrease in blood pressure during sleep.
- Increased Cardiovascular Risk: Non-dippers are at higher risk for heart disease, stroke, and other cardiovascular events due to the continuous strain placed on the heart and blood vessels throughout the day and night.
- Association with Hypertension: Non-dippers are often diagnosed with hypertension or other cardiovascular conditions. The lack of dipping is considered an indicator of poor cardiovascular health and can signal damage to the heart or blood vessels.
Non-dipping patterns are especially common in individuals with certain medical conditions, such as diabetes, chronic kidney disease, and obstructive sleep apnea. The absence of a nocturnal dip may also be seen in older adults, individuals with high levels of stress, and those with an unhealthy lifestyle.
Factors Influencing Dipping and Non-Dipping Patterns
Several factors contribute to whether an individual is a dipper or a non-dipper. These factors can be broadly classified into lifestyle-related, medical, and environmental categories. Understanding these factors can help individuals manage their risk and maintain healthy blood pressure levels.
- Age: As individuals age, the prevalence of non-dipping patterns increases. Older adults are more likely to have impaired circadian rhythms, leading to less pronounced reductions in blood pressure at night.
- Hypertension: People with high blood pressure, or hypertension, are more likely to be non-dippers. Persistent high blood pressure, particularly if not well-controlled, can prevent the heart from reducing its workload during sleep.
- Diabetes: Individuals with diabetes are at a higher risk of being non-dippers. This is partly due to the impact of diabetes on blood vessels and the autonomic nervous system, which can disrupt normal blood pressure regulation.
- Chronic Kidney Disease: Non-dipping is common in individuals with chronic kidney disease. The kidneys play a crucial role in regulating blood pressure, and when they are not functioning properly, this regulation can be impaired.
- Obstructive Sleep Apnea (OSA): Obstructive sleep apnea is a condition in which breathing repeatedly stops and starts during sleep. This can lead to surges in blood pressure during the night, disrupting the normal dipping pattern.
- Lifestyle Factors: Sedentary lifestyle, poor diet, smoking, excessive alcohol consumption, and chronic stress can all contribute to the development of non-dipping patterns. These factors increase overall cardiovascular risk and can interfere with the body’s ability to regulate blood pressure.
- Medications: Certain medications, particularly those used to treat high blood pressure, can influence dipping patterns. Some antihypertensive medications are more effective during the day than at night, potentially contributing to a non-dipping pattern.
Health Risks Associated with Non-Dipping
The absence of a nocturnal dip in blood pressure is associated with a variety of health risks, particularly cardiovascular complications. Non-dippers are at greater risk for the following conditions:
- Heart Disease: Non-dippers have a higher likelihood of developing coronary artery disease, heart failure, and other heart-related issues. The continuous strain on the heart can lead to structural changes, such as left ventricular hypertrophy, which increases the risk of heart disease.
- Stroke: Non-dippers are at higher risk for ischemic stroke, which occurs when blood flow to the brain is blocked. Elevated nighttime blood pressure can damage the blood vessels in the brain, making a stroke more likely.
- Kidney Disease: Since blood pressure regulation is closely linked to kidney function, non-dippers are more likely to experience kidney damage or chronic kidney disease.
- Diabetic Complications: Individuals with both diabetes and a non-dipping blood pressure pattern are at particularly high risk for cardiovascular events and diabetic complications. Elevated nighttime blood pressure can worsen damage to blood vessels, nerves, and organs in diabetic patients.
- Cognitive Decline: Research suggests that non-dippers may be at higher risk for cognitive decline and dementia. The continuous high blood pressure, especially at night, may contribute to reduced brain perfusion and subsequent cognitive impairment.
Monitoring Blood Pressure and Diagnosis
Accurately diagnosing whether an individual is a dipper or non-dipper requires continuous blood pressure monitoring, typically over a 24-hour period. This process is known as ambulatory blood pressure monitoring (ABPM). ABPM allows healthcare providers to track blood pressure during both daytime and nighttime hours, providing a comprehensive picture of the patient’s blood pressure profile.
Key Benefits of ABPM:
- Identification of Nocturnal Patterns: ABPM helps identify whether the individual is a dipper or non-dipper by measuring nighttime blood pressure. This can guide treatment decisions and risk assessment.
- Improved Hypertension Management: ABPM provides more accurate information about blood pressure fluctuations, leading to better-informed treatment strategies.
- Risk Stratification: Identifying non-dippers allows healthcare providers to stratify patients by risk and prioritize those who may benefit from more intensive monitoring or treatment.
Management and Treatment Strategies for Non-Dippers
For non-dippers, managing blood pressure and reducing cardiovascular risk often requires a combination of lifestyle changes and medical interventions. Below are some strategies to consider.
- Lifestyle Modifications:
- Regular Physical Activity: Engaging in regular exercise can help regulate blood pressure and improve circadian rhythms.
- Healthy Diet: A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, can support blood pressure management.
- Stress Management: Reducing stress through mindfulness, relaxation techniques, and adequate sleep can improve overall cardiovascular health.
- Limit Alcohol and Tobacco Use: Reducing or eliminating alcohol and tobacco can lower the risk of developing a non-dipping pattern and improve heart health.
- Medication Adjustments:
- Antihypertensive Medications: For individuals with hypertension, taking blood pressure medications at night, rather than in the morning, can help restore a dipping pattern. This is particularly effective with long-acting antihypertensives.
- Medications for Associated Conditions: Treating conditions like diabetes, kidney disease, or sleep apnea can help improve blood pressure regulation and reduce the risks associated with non-dipping.
- Treatment of Sleep Apnea: For individuals with obstructive sleep apnea, using a continuous positive airway pressure (CPAP) device during sleep can help reduce blood pressure fluctuations and restore a dipping pattern.
- Regular Monitoring: Non-dippers may benefit from more frequent blood pressure monitoring to ensure that their condition is well-controlled. Home blood pressure monitors and regular check-ups with healthcare providers can be crucial for managing long-term risks.
Conclusion
Understanding the difference between dippers and non-dippers provides important insight into cardiovascular health. While dippers experience the normal, protective decrease in blood pressure during sleep, non-dippers are at greater risk for cardiovascular events due to the continuous strain on their cardiovascular system. Identifying non-dipping patterns through ambulatory blood pressure monitoring is essential for guiding treatment and managing risks.
Lifestyle modifications, medication adjustments, and treatment of underlying conditions can help non-dippers restore healthier blood pressure rhythms and reduce their risk of heart disease, stroke, and other complications. With the right approach, individuals can manage their blood pressure and protect their long-term health.
FAQs
1. What is the difference between a dipper and a non-dipper in blood pressure?
A dipper is someone whose blood pressure decreases by 10-20% at night compared to daytime values, while a non-dipper experiences little or no decrease in blood pressure during sleep.
2. How is dipping and non-dipping identified?
Dipping and non-dipping patterns are identified through ambulatory blood pressure monitoring (ABPM), which measures blood pressure continuously over a 24-hour period, including both daytime and nighttime readings.
3. What causes a person to be a non-dipper?
Factors such as age, hypertension, diabetes, chronic kidney disease, obstructive sleep apnea, stress, and unhealthy lifestyle choices can all contribute to non-dipping blood pressure patterns.
4. Are non-dippers at a higher risk of heart disease?
Yes, non-dippers are at a higher risk for heart disease, stroke, kidney disease, and other cardiovascular complications because their blood pressure does not decrease during sleep, placing greater strain on the heart and blood vessels.
5. Can non-dipping be treated or managed?
Yes, non-dipping can be managed through lifestyle changes, medication adjustments, treatment of associated conditions, and monitoring. In some cases, taking blood pressure medications at night can help restore a dipping pattern.
6. Is non-dipping more common in certain medical conditions?
Non-dipping is more common in individuals with hypertension, diabetes, chronic kidney disease, and obstructive sleep apnea. It is also more likely to occur in older adults and those with an unhealthy lifestyle.